Varicose veins are abnormal dilated veins due to the weakening of the vein walls or/and due to the incompetent (leaky) valves.
How Varicose Veins occur?
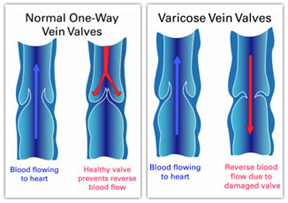
Normal veins have the job of taking blood back to the heart. From the legs the flow of venous blood occurs against gravity by the action of muscles when we walk or exercise. Veins have one-way valves in them to overcome the effects of gravity. When the walls of the leg veins lose their elasticity and the valves stop functioning properly (becomes leaky), blood can flow backwards and pool in the superficial leg veins, causing the veins to swell and become varicose.
Venous Insufficiency most commonly manifests as varicose veins, swollen and aching legs, skin changes or leg ulcers. It is quite common for patients to have venous insufficiency without having visible signs of varicose veins.
Risk factors for varicose veins
Factors that can increase your chance of developing varicose veins include:
- Increasing age
- Pregnancy
- Family history of varicose veins
- Overweight
- Female
- Standing still or sitting for long periods of time
Symptoms of varicose veins
Varicose veins are a cosmetic concern for many people, appearing as visible blue or purple veins under the skin or twisted, swollen veins that are like cords on the legs. Spider veins (tiny red or blue veins that resemble a spider web) are a smaller type of varicose vein.
Initially, varicose veins are usually painless. Over time they can cause symptoms and signs such as:
- Aching pain in the legs, especially when standing and walking
- Cramps in the legs
- Restless legs
- Swelling of the legs and feet
- Discoloured skin in the area around the varicose veins
- An itchy rash (varicose eczema).
- Ulcers near the ankle
- Bleeding from the varicose veins
Diagnosis and tests

Doctors can often diagnose varicose veins by examining the veins in the legs. Your doctor may recommend having a colour duplex ultrasound for the detailed examination of both deep and superficial veins. Ultrasound examination is important to check for blood clots and whether the valves in the veins are functioning properly.
Treatment for varicose veins
The aims of treatments
- To ease symptoms – aching, cramps, swelling, itching, burning etc.
- Improve appearance
- Prevent complications such as leg ulcers, bleeding, skin discolouration, venous eczema etc.
Types of treatment
Life style modification
- Regular exercise that improves the muscle tone in your legs
- Losing weight if you are overweight
- Avoiding wearing clothes that are tight around the legs, groin and waist
- Keeping your legs elevated when you are sitting
- Avoiding standing still for prolonged periods
Compression stockings
Doctors often suggest wearing elasticised compression stockings as the initial treatment for varicose veins. These stockings create gentle pressure up the leg to prevent blood from pooling in the veins. They can help with leg pain and swelling.
Varicose veins that don’t respond to life style modification and compression stockings need further treatment.
Sclerotherapy
Sclerotherapy is a form of treatment that involves injecting the varicose veins with a chemical solution that irritates and scars the vessel walls, making them stick together. This blocks off the veins, so that they can’t carry blood and so are less visible under the skin.
Ultrasound Guided Sclerotherapy
This is injecting deeper veins with sclerosant under ultrasound guidance. This is used to treat bigger veins situated deep under the skin, which is normally not visible outside.
Endovenous ablation therapy (Radiofrequency/ Laser ablation therapy)
These are newer techniques used to close off large varicose veins. These treatments apply heat to the inside of the veins, which collapses them and seals them shut. This is relatively painless procedure and the patient can get back to normal activities soon after the procedure. The risk of DVT is much lower than surgical procedures. This is normally done as an office procedure without any need of hospitalisation.
Surgery
There are several types of surgery that can be performed to treat varicose veins.
- Ambulatory phlebectomy removes varicose veins in the lower leg through a series of small skin punctures. It is usually used for small veins that are close to the skin surface.
- Vein stripping and ligation (tying shut and removing longer veins through small cuts in the skin) is usually used to treat more severe cases of varicose veins.